FEATURE
29 November 2018
The HIV-positive caregivers working to end AIDS in Africa
Dotty Nyambok is an HIV Counsellor at the Embakasi Health Centre in Nairobi, Kenya. She is halfway through her list of patients when two girls walk into her tent.
Helima, 18, is here because she suspects she’s contracted HIV from her boyfriend, and her friend Winny has come to support her.
Dotty begins a familiar ritual: She unwraps a sterilised needle, pricks Helima’s finger and drops blood onto a test strip. Then she sets the timer. 15:00, 14:59, 14:58…
While they wait, Dotty asks Helima what she thinks will happen if she tests positive. With grim confidence, she answers, she will die.
That’s when Dotty shares something of herself. It’s information she reveals when she senses someone is in desperate need of kindness and hope.
“I’m HIV-positive,” Dotty says. “So when you have HIV you will continue living, because you will take your medication.”
The girls exchange surprised, shy smiles in the tent at Embakasi, a facility whose HIV treatment services have been supported by Apple’s (RED) partnership since 2012.
Since its founding by Bono and Bobby Shriver, (RED) has raised more than $600 million to support the Global Fund to Fight AIDS, Tuberculosis and Malaria, $200 million of which has come from its partnership with Apple, the organisation’s largest corporate donor.
Last year, Kenya had 53,000 new cases of HIV. Young women are infected at twice the rate as young men. As high as these numbers seem, they’re a vast improvement from years ago.
In 2000, a staggering 9.3 percent of all adults in Kenya were HIV-positive. At the same time, because the drugs were in short supply, World Health Organization guidelines stipulated that lifesaving antiretrovirals (ARVs) should only be administered once a patient’s CD4 count, which measures immune system health, fell below a very low mark. It meant patients had to be extremely sick to access ARVs, and for many, that was too late.
5:27, 5:26, 5:25…
That grim landscape was recent history when Dotty discovered she was pregnant in 2007, at age 19. During a prenatal visit, a clinician told Dotty she was HIV-positive, and pointed her to a treatment clinic two hours away. There was no counselling, no compassion, and no follow-up.
The experience left her traumatised and in denial — she didn’t tell anyone about her status and didn’t seek treatment.
Dotty’s son died in her arms at just six weeks old. He was buried in a cooking oil box — the smallest they could find.
A few months later, Dotty went to the Embakasi Health Centre.
It’s one of thousands of facilities in Kenya and seven other countries in Sub-Saharan Africa that began receiving support from the Global Fund in 2002.
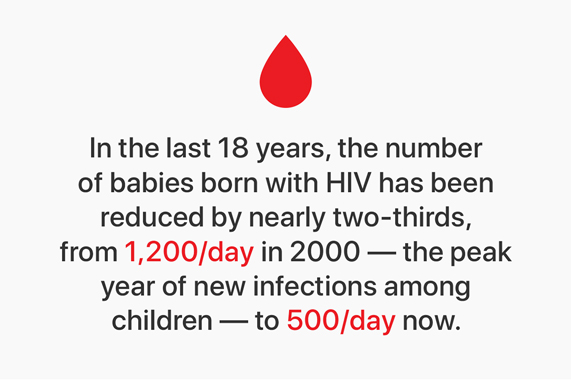
The Global Fund has helped to radically change access to HIV treatment, and provides 17.5 million people with ARVs — now available from the moment they test positive. As a result, Kenya has seen a 52 percent drop in new HIV infections since 2000. As of last year, just 4.8 percent of all adults were HIV-positive.
“I decided to do counselling because I really don’t want what happened to me to repeat itself.”
In 2009, Embakasi opened a special Comprehensive Care Clinic (CCC) for HIV patients that distributes ARVs, made possible largely from Global Fund grants.
“The Global Fund and (RED) have made a huge impact in the lives of HIV-positive patients,” says Robina Anene Muli, who runs the Embakasi Health Centre. “Especially when it comes to testing kits, ARVs and other drugs — they provide 80 percent of our supplies and funding.”
3:13, 3:12, 3:11…
During her first year at Embakasi, Dotty was introduced to the Mentor Mothers, a group of peer educators who are HIV-positive and have given birth to HIV-negative babies after taking ARVs. The group was created as part of the CCC expansion, with Global Fund grants.
After a few months of treatment, Dotty found out she was pregnant again.
On November 7th, 2009, Dotty gave birth to a healthy baby boy. “Now I had a reason to live,” she says. “Because of Morgan. He saved my life.”
When Morgan was six months old, Dotty applied to be a Mentor Mother at Embakasi.
“I decided to do counselling because I really don’t want what happened to me to repeat itself,” says Dotty. “My purpose is to touch a heart — and if I diagnose someone I feel like we are then attached.”
In many facilities, HIV-positive peer educators like Dotty are changing the way people live with HIV.
“Peer educators are a vital piece of the most effective HIV treatment programs,” says Luisa Engel, Chief Impact Officer at (RED). “Their work ensures lifesaving information reaches the people who need it most, and they act as a powerful force against stigma.”
Three years ago, Dotty started a new role at Embakasi, as an HIV Testing Counsellor. Sometimes she takes an HIV test in front of her patients, to prove she has the virus and to show them that a full and vibrant life is possible.
“I would like to see a different perception about HIV,” says Dotty. “And that’s what I hope to do when I disclose my status.”
:03, :02, :01…
Back in Dotty’s tent, Helima’s results are ready. She places the test strip in between examples of what a positive and negative result look like.
“Tell me what you see and what it means,” says Dotty.
“Negative,” says Helima. In an instant, the tension dissolves. After a chat about how to protect themselves, Dotty sends the girls off with warm goodbyes.
On Dotty’s walk home that night, she picks up some meat to cook for dinner on the hotplate in the one-room apartment she and Morgan, now nine years old, share.
After dinner, at 7:58 p.m., an alarm on Dotty’s phone sounds. It signals the start of a ritual they have repeated every night for the last two years — ever since Morgan was old enough to understand his mom’s illness.
Morgan walks over to a small dresser, pulls out a bottle of pills and carefully taps one out. He hands the ARV to his mother, who swallows it with water.
These are the frontlines of the war against AIDS in Africa. And this is how it is won, one expression of love, one act of kindness, at a time.
Images of the Embakasi Health Centre